Retina
Diabetic Retinopathy
Diabetic retinopathy is a diabetic eye disease that causes damage to the blood vessels within the retina. The National Eye Institute reports it as the leading cause of blindness in U.S. adults. The condition is progressive, with symptoms beginning subtly and advancing over time. In fact, the earliest stage, known as mild non-proliferative retinopathy, is often symptom-free and identifiable only by a comprehensive dilated eye exam. This exam is especially important for diabetics at least once yearly.

As diabetic retinopathy progresses into moderate and severe non-proliferative retinopathy or proliferative retinopathy, symptoms may include:
- Blurred vision
- “Floaters,” (dark specs and lines that appear to float within the field of vision)
- Difficulty seeing at night
- Dark or missing spots in the central field of vision
- Partial or total blindness
Any new symptoms that arise require immediate attention by an eye care professional. A comprehensive eye exam can measure the pressure within the eye and examine it for retinal swelling, nerve damage and changes in blood vessels. If diabetic retinopathy is diagnosed before it has fully progressed, treatments are available to help preserve vision.
Laser Treatment – Scatter laser treatment and focal laser treatment are surgeries performed in an ophthalmologist’s office to shrink abnormal blood vessels or prevent retinal fluid leakage. A laser is used to carefully “burn” the areas around abnormal blood vessels or the macula that could otherwise cause loss of sight.
Vitrectomy – This procedure is performed in a hospital to remove blood that has leaked into the center of the eye. A vitrectomy can restore sight to the visual field.
Only an eye health professional can diagnose diabetic retinopathy. Individuals with diabetes are at the highest risk for developing the disease, although other risk factors include being pregnant, Hispanic or African American, as well as having high blood pressure or high cholesterol. Annual eye examinations are essential for preventive eye health – especially in these risk groups.
Flashes and Floaters
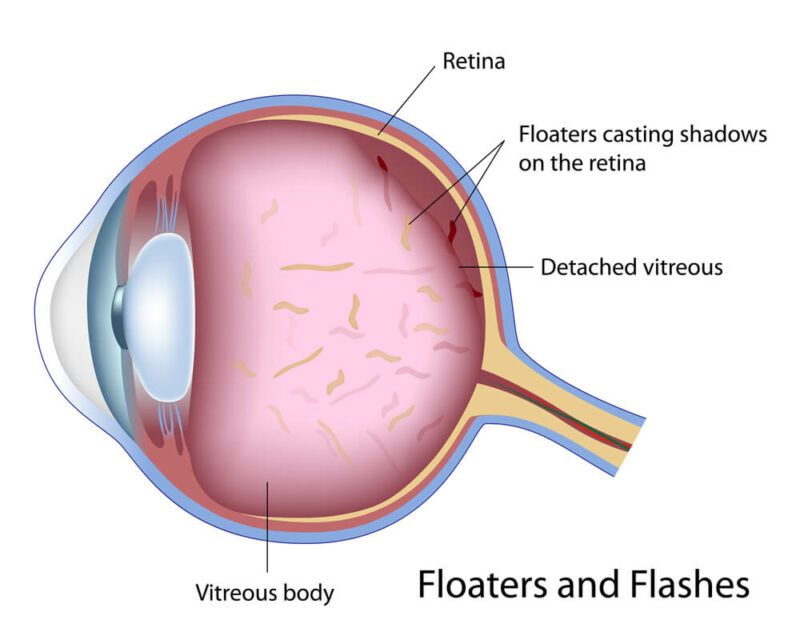
Floaters are easily identified by their ability to move within the field of vision. They can come in many shapes, including dots, lines and “cobwebs.” Eye floaters are seen best when looking at a blank background, and they may occur anywhere within the field of vision, including the central and peripheral vision. Though many mistake them for being objects on top of or in front of the eye, they are actually the result of an accumulation of cells within the eye.
Flashes are unlike floaters, in that they appear as rapid bursts of light. They may be more easily noticed in dim lighting. Both floaters and flashes may develop slowly due to age-related posterior vitreous detachment, or they may develop suddenly – potentially signifying a retinal tear.
Vitreous Detachment – A condition in which the vitreous gel retracts from the back of the eye. It is very common in individuals over age 40 and especially in those who are nearsighted, have undergone eye surgery or experienced an eye trauma.
Retinal Tear – A serious condition often caused when vitreous detachment results in a tear in a weakened retinal wall. Retinal tears have a high chance of leading to a complete retinal detachment if left untreated. Tears found early can be surgically treated to prevent detachment and total vision loss.
The only way of determining whether floaters are the evidence of a retinal tear or detachment is by visiting an ophthalmologist for an eye exam. Most floaters are not cause for alarm and will fade over time. But some – especially those that develop suddenly – could be a sign of future vision loss. It is important to visit an ophthalmologist at the first sign of an increase in floaters or the onset of sudden flashes of light.
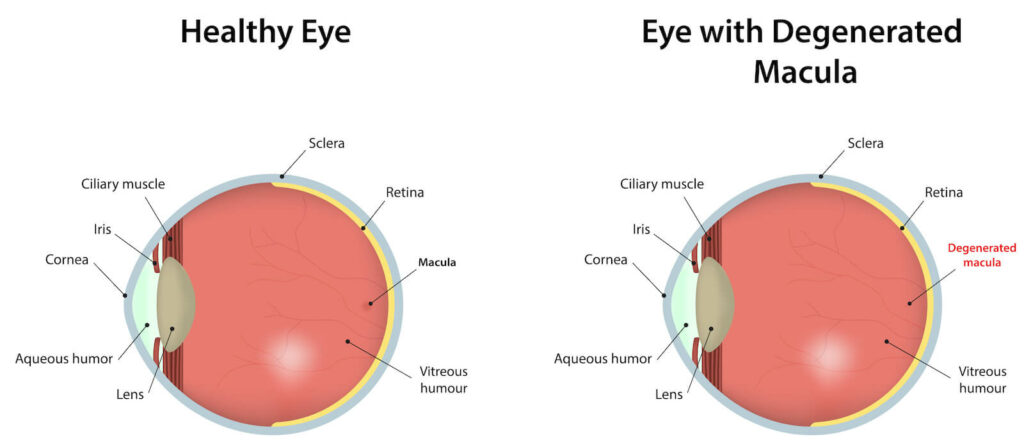
Macular Degeneration
Macular degeneration is an eye disease that occurs when the eye’s macula begins to deteriorate, leading to blurred vision and partial vision loss. It is mostly associated with aging and is the leading cause of vision loss among people over age 60. Aside from age, there are specific risk factors identified with an increased risk of developing macular degeneration. They include being Caucasian, being obese, using tobacco products and having high blood pressure or cholesterol.
Wet Macular Degeneration
Wet macular degeneration is the least common form of the eye disease and is identified by the presence of abnormal blood vessels beneath the macula. As the blood vessels begin to leak, fluid distorts vision, creating blind spots and indistinct lines. Eventually, scarring occurs around the blood vessels, which results in a permanent loss of central vision.
Dry Macular Degeneration
Dry macular degeneration is the most common version of the disease and is caused by an aging of the macula rather than the growth of abnormal blood vessels. Dry macular degeneration usually begins with minor symptoms, such as the presence of yellow drusen within the eye. As the drusen multiply and expand, vision becomes darker or distorted. Over time, blind spots may develop and a minority of patients may eventually develop the wet form of the disease.
Coping with Macular Degeneration
Macular degeneration can be a very frustrating disease, as patients suffering with it may have trouble performing routine tasks, reading a book, operating a vehicle or even recognizing faces. Although there is currently no cure, the disease can be managed and its progress slowed – especially when it is detected in its earliest stages.
Dry macular degeneration is age-related and may be helped with regular consumption of certain vitamins. We recommend Macutene Protect to support optimal macular health using ultra premium ingredients that are made in the U.S.A., this is available at www.eyecheck.com
For patients who have wet macular degeneration, anti-angiogenesis medications may be effective in preventing the growth and formation of new blood vessels beneath the macula. These drugs usually slow the progression of macular degeneration and in some cases helps patients regain a portion of previously lost central vision. Ophthalmologists also use laser therapy to damage and destroy abnormal blood vessels within the eye.
Routine eye exams are essential to maintaining good eye health and diagnosing eye diseases like macular degeneration before they have a chance to progress. Anyone experiencing dark or blurry vision or reduced color perception should see an eye doctor as soon as possible, as these symptoms could be signs of macular degeneration.
Retinal Detachment
Retinal detachment is an uncommon, but serious eye condition that occurs when the retina separates from the back of the eye. This condition is very serious and can result in a permanent loss of vision if not quickly diagnosed and treated by an ophthalmologist.
Usually, retinal detachment occurs as the result of a retinal tear. These tears occur when the vitreous gel liquefies and begins to separate from the back of the eye – a condition that is normal after age 40. But when the retinal tissue is weak, a tear can occur causing the newly liquefied gel to leak and collect under the retina.

Symptoms of Retinal Detachment
Unfortunately, there is no pain or discomfort to signify the detachment of the retina. Because the condition is not uncomfortable, it often goes undiagnosed and untreated until it is too late to preserve vision. However, there are some tell-tale signs that retinal detachment is occurring, including the sudden appearance of floaters or flashes of light. A darkening or “graying” of the peripheral vision is also an indicator of a detached retina.
Although retinal detachment can occur to anyone, it is more common among individuals with certain risk factors. They include:
- Being over age 40
- Having a family history of retain detachment
- A previous eye trauma, injury, or surgery
- The presence of an eye disease
- Myopia (nearsightedness)
- Previous retinal detachment
Anyone experiencing the symptoms of retinal detachment should seek emergency help from an ophthalmologist. Early identification and treatment can prevent vision loss or preserve remaining vision.
Treatment ofRetinal Detachment
Retinal detachment found early enough can be surgically treated. Laser surgery and cryopexy (freezing) are both methods of creating scarring that helps close retinal tears and secure the retina to the surrounding tissue and eye wall. In some cases, it may also be necessary to use simultaneous procedures, such as draining and replacing the vitreous fluid within the eye or injecting gas into the eye to help seal retinal tears and encourage the absorption of fluid that has collected beneath the retina.
